TU Delft researcher Joan Gallego developed a method to produce red blood cells, paving the way to donor-free blood transfusions. Clinical trials should begin by 2025.
There is a worldwide shortage of donor blood. Affordable production of red blood cells in tanks opens the window to donor-free blood transfusions. (Photo: Nguyen Hiep / Unsplash)
Joan Gallego conducted his PhD research on ‘process development for cultured red blood cell production’ in TU Delft’s Bioprocess Engineering section (Faculty of Applied Sciences). His goal was to make the production of blood easier, more scalable and affordable, so that we can stop relying solely on donors and, ultimately, produce blood ‘on demand’, as he says.
“It is a breakthrough for us,” says Marieke von Lindern, a researcher at Sanquin, a Dutch blood bank which initiated the research and collaboration with TU Delft. “We have made a huge leap forward thanks to Joan’s PhD research. I never thought this would be possible. There is a worldwide shortage of donor blood, which is why we need cultured blood. If we are successful, it’d be a huge help for many.”

One transfusion dose requires 25,000 petri dishes. (Photo: Joan Gallego)
Rare blood
The idea to culture cells for blood transfusions is relatively new, but motive behind it is very clear. At the moment, everyone in the world is dependent on the availability of donated blood. This can be problematic in general, but causes serious issues for patients with rare blood types in particular.
“There are many patients for whom we struggle to find a transfusion unit,” says Von Lindern. “For some, we need to import blood from America or even Australia, because it simply cannot be found anywhere else.” This shortage means that some patients cannot get optimal care. “There are people who cannot have the surgery they need because there isn’t enough blood for them.”
Producing cultured red blood cells would offer solutions to these and other challenges, and researchers at Sanquin have already been working on ‘manufacturing blood’ for many years. They succeeded too, but only at a very small scale. “We were able to culture about 10 microliter of cells in a petri dish,” explains Von Lindern. Not quite enough, as you’d need about 25,000 dishes to produce a single transfusion unit – while most patients require more than one unit (500 ml which consists of about 250 ml of red blood cells and 250 ml of plasma)
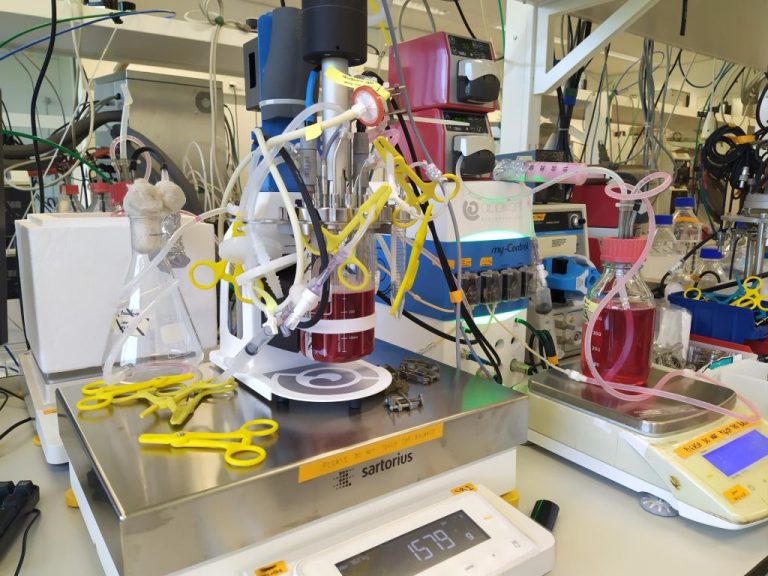
Gallego scaled production up from petri dishes to bioreactor, such as the one in this lab. (Photo: Joan Gallego)
From millilitres to litres
“For this system to work, a lot of manual work, time and space would be needed. It was not a scalable solution,” says Joan Gallego. The goal of his PhD project was to make the process more scalable – and more affordable, as the production would otherwise amount to roughly EUR 400,000 per transfusion unit.
Suddenly the researchers could move from millilitres to litres
Gallego replaced petri dishes with stirred tank bioreactors, which are standardly used for the large-scale production of biopharma therapeutics. It turned out that bioreactors were a great alternative to the traditional small dishes. Suddenly, the researchers could move from working with millilitres to working with litres. “We successfully tested the process with three litre reactors, but the bioreactors can also hold hundreds of litres. This solution therefore saves a lot of time and manual labour,” explains the PhD candidate.
More good news followed, as Gallego found out that bioreactors were suitable for both stages of culturing red blood cells. “The first phase of the process is proliferation, where you try to produce as many cells as possible,” explains the scientist. “You start with a small number of cells, putting erythroblasts [precursor cells in red blood cell formation, Ed.] with fresh media into the reactor. You keep adding fresh media, such as the protein needed to deliver iron to the cells, and you keep supplying oxygen throughout the process. The second phase is the differentiation phase when the cells transform into red blood cells. I found out that we could safely use bioreactors for both phases.”
This bioprocess technology is already a big step forward, but Gallego’s research went even further. He was able to replace highly expensive growth factors that are normally needed for the cell culture and substitute it for a cheap and bio-compatible molecule: iron-loaded deferiprone. This is a much cheaper solution, saving hundreds of thousands of euros per transfusion unit.
Clinical trial
Although many challenges still lie ahead, Joan Gallego’s work offers unprecedented possibilities, says Marieke von Lindern. ‘‘Before, we just worked in small dishes. Now we can move to large reactors – we didn’t dare to even think of that before. We will continue the research and strive to make the method more cost effective. Even though we can’t produce full transfusions yet, we now know the route.”
Sanquin is planning a clinical trial using the newly developed method. “We first need to get the ethical approval, but we’d like to start the clinical trial in 2025,” says Von Lindern. “We want to then do a 10% transfusion, meaning a mini transfusion equalling 10% of a regular one. We hope to produce the cells and test their stability in volunteers.”
Donor-free blood in 10 years’ time
How long will it be until blood transfusions can be ‘made on demand’? Von Lindern is hopeful, she says. “I started working at Sanquin in 2010, and the first thing they told me was: you have to start producing red blood cells. At that time, I wasn’t sure such a thing was even possible. Now I believe that we can produce real transfusion units to help patients in about 10 years’ time.”
- Joan Gallego defended his doctoral dissertation Friday, 10 November 2023.
- Read also: Safe and affordable red blood cells without donors (TU Delft communication)
Do you have a question or comment about this article?
michaela.nesvarova@gmail.com


Comments are closed.