Two TU Delft researchers suspect a link between low indoor air humidity and the infection rate. If this is the case, the number of infections will drop in spring.
Spring on campus in 2019. (Photo: Marjolein van der Veldt)
They sought contact with the press in recent months because they had an urgent message about corona infections. Their message was crystal clear, namely that dry indoor air favours Covid-19 infections. The regional press and the ‘Telegraaf’ newspaper responded to their ‘cry for help’. After Maurice de Hond’s aerosols campaign and the call for more ventilation in classrooms, the warning about the indoor climate sounded familiar. Yet their story is different.
Dr Geert Keetels (Particle Transport at 3mE) and Prof. Bas van de Wiel (Atmospheric Physics at CiTG) put the emphasis on humidification in addition to ventilation. Dry air is advantageous to viruses. Ventilation with cold outside air makes the air inside drier, and dry air increases the risk of infection. The ‘Telegraaf’ recommended hanging up laundry inside and the next day humidifiers were sold out everywhere.
(Illustration: Keetels en Van de Wiel)
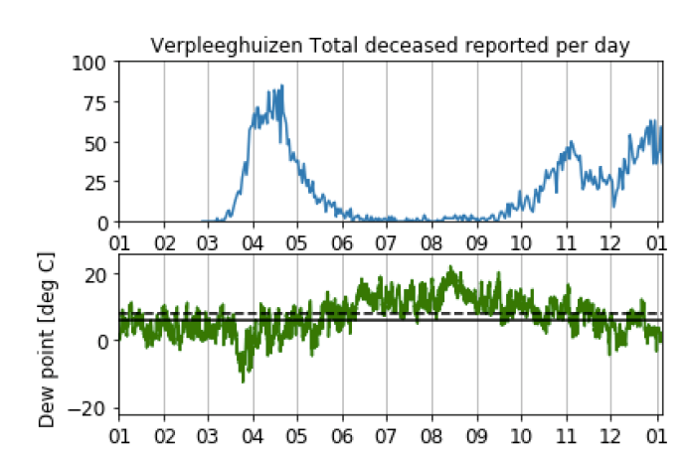
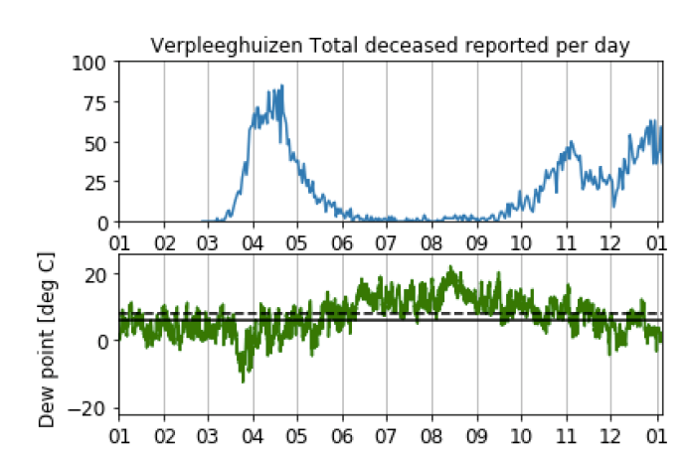
An intriguing graph marked the beginning of their campaign. The top line shows the number of Covid-19 deaths per day and the bottom line the indoor humidity. The lines seem to mirror each other. At indoor humidity levels of 40% or more, the number of infections drops; at lower humidity levels, it rises.
Dry threat
What is going on? As the mercury drops, the outside air contains less moisture and the air becomes drier when heated. Evaporation causes exhaled aerosols (suspended particles of moisture) to shrink in the dry environment and they float around for longer and enter the lungs more deeply. In addition, the immune system is often already under pressure in winter due to irritations and dehydration.
An earlier American study into the effect of humidification in schools and the number of flu infections showed a 30-50% reduction in the number of viruses and the number of infections. Humidification was potentially ‘an important non-pharmaceutical intervention’ according to the study.
The critical threshold seems to be an indoor relative humidity of 40%. An indoor temperature of 20 degrees Celsius means a ‘dew point’ of 6 degrees Celsius or more for the outdoor air. The dew point (in Dutch) is the temperature at which the relative humidity is 100%.
Testing
How can the supposed relationship between humidity and infections be proven? One way is a retrospective study that Keetels and Van de Wiel would like a graduate student to conduct: does the use or non-use of humidifying devices affect the number of sick notes in comparable institutions? Does air humidification in nursing homes affect the number of Covid-19 or flu infections? That is what comparative studies should show.
Another experiment will happen naturally. As the outside temperature rises, so does the relative humidity indoors. From about 12 degrees outside, indoor humidity remains above the critical limit of 40%. According to Keetels and Van de Wiel’s hypothesis, the number of infections will then decrease. Let spring come. And quickly.
Do you have a question or comment about this article?
j.w.wassink@tudelft.nl


Comments are closed.